Introduction: The Power-Risk Paradox of BFRT
Blood Flow Restriction Training (BFRT) represents one of the most significant advances in exercise science and rehabilitation in the past two decades. By enabling muscle hypertrophy and strength gains with loads as low as 20-30% of one-repetition maximum (1RM), BFRT offers unprecedented opportunities for populations who cannot tolerate traditional high-load training—post-surgical patients, individuals with osteoarthritis, elderly populations, and athletes managing high training volumes.
However, this remarkable efficacy comes with a responsibility: BFRT creates a unique physiological stress environment that, while generally safe when applied correctly, requires rigorous adherence to evidence-based protocols. The same mechanisms that drive its benefits—metabolic stress, cellular swelling, and partial vascular occlusion—also introduce potential risks if proper screening, individualization, and monitoring are not implemented.
This comprehensive guide provides medical professionals, physical therapists, athletic trainers, and qualified fitness practitioners with the clinical knowledge necessary to implement BFRT safely and effectively. We cover:
- Scientific foundation and mechanisms of adaptation
- Documented adverse events and their incidence rates
- Absolute and relative contraindications for BFRT
- Risk stratification and screening protocols
- Evidence-based prescription parameters
- Real-time monitoring and stop criteria

The BFRT Foundation: Scientific Efficacy & Mechanisms
Before addressing safety protocols, it is essential to understand why BFRT works. This scientific foundation contextualizes the physiological stress we are managing and explains why precision in application matters.
Evidence-Based Efficacy
Multiple systematic reviews and meta-analyses have established that low-load BFRT (20-40% 1RM) produces muscle hypertrophy and strength gains comparable to traditional high-load resistance training (70-85% 1RM). Key findings include:
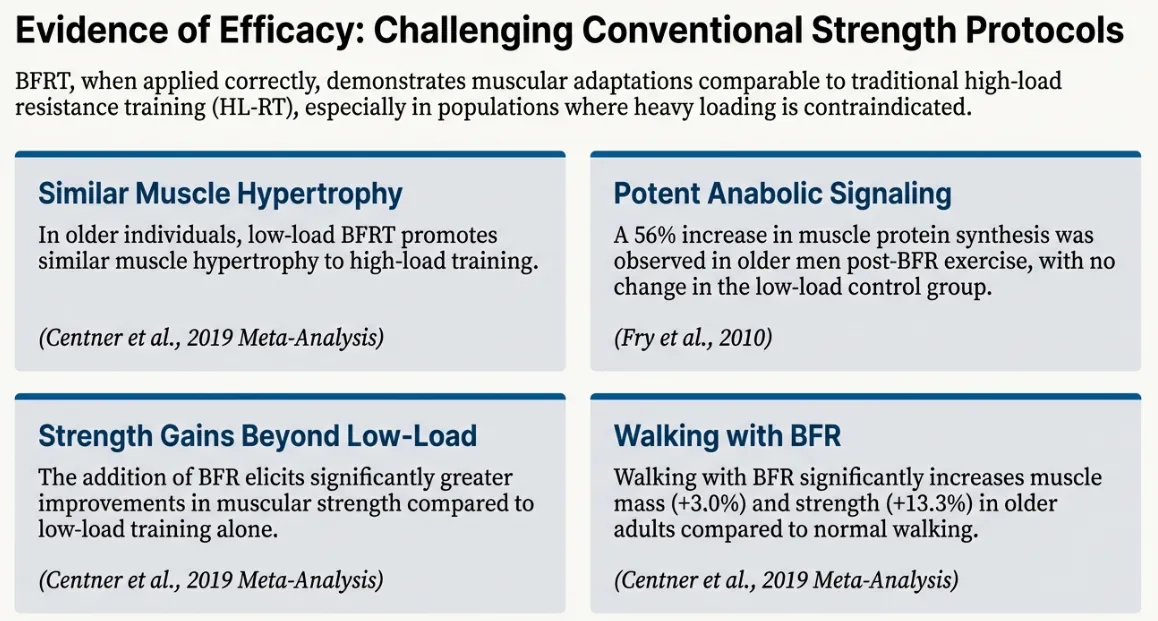
- Muscle Hypertrophy: Low-load BFRT produces similar increases in muscle cross-sectional area and volume compared to high-load training
- Strength Gains: Improvements in 1RM strength, though slightly less than high-load training in trained populations
- Anabolic Signaling: Activation of mTORC1 pathway and increased muscle protein synthesis rates
- Clinical Applications: Effective for post-surgical rehabilitation, sarcopenia prevention, and low-intensity aerobic exercise enhancement
The Adaptation Process
BFRT triggers a cascade of physiological mechanisms that work synergistically to produce muscle growth:
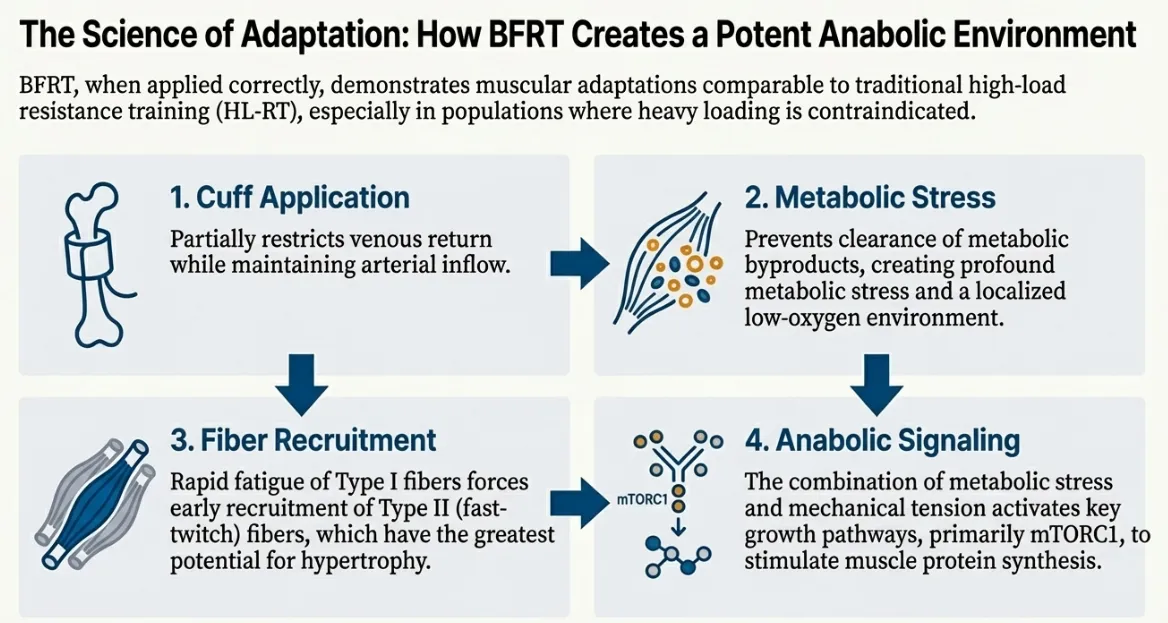
- Cuff Application & Vascular Occlusion: Partial restriction of venous return while maintaining arterial inflow creates a pooling effect in the working muscle
- Metabolic Stress Accumulation: Trapped metabolic byproducts (lactate, H+, inorganic phosphate) create a hypoxic, acidic environment that mimics high-intensity exercise
- Accelerated Fiber Recruitment: Rapid fatigue of Type I fibers forces early recruitment of Type II fast-twitch fibers, even at low loads
- Anabolic Signaling: Combined mechanical tension, metabolic stress, and cellular swelling activate growth pathways (mTORC1) and satellite cell proliferation
This powerful adaptation process is precisely why safety protocols are non-negotiable. We are inducing a controlled physiological stress that requires careful management.
Understanding the Risks: The BFRT Paradox
The same physiological mechanisms that make BFRT effective also introduce potential risks. While serious adverse events are rare when proper protocols are followed, understanding these risks is essential for informed clinical decision-making.
Documented Adverse Events
Systematic reviews of BFRT research have documented various adverse events, though their incidence is generally low in controlled clinical settings:
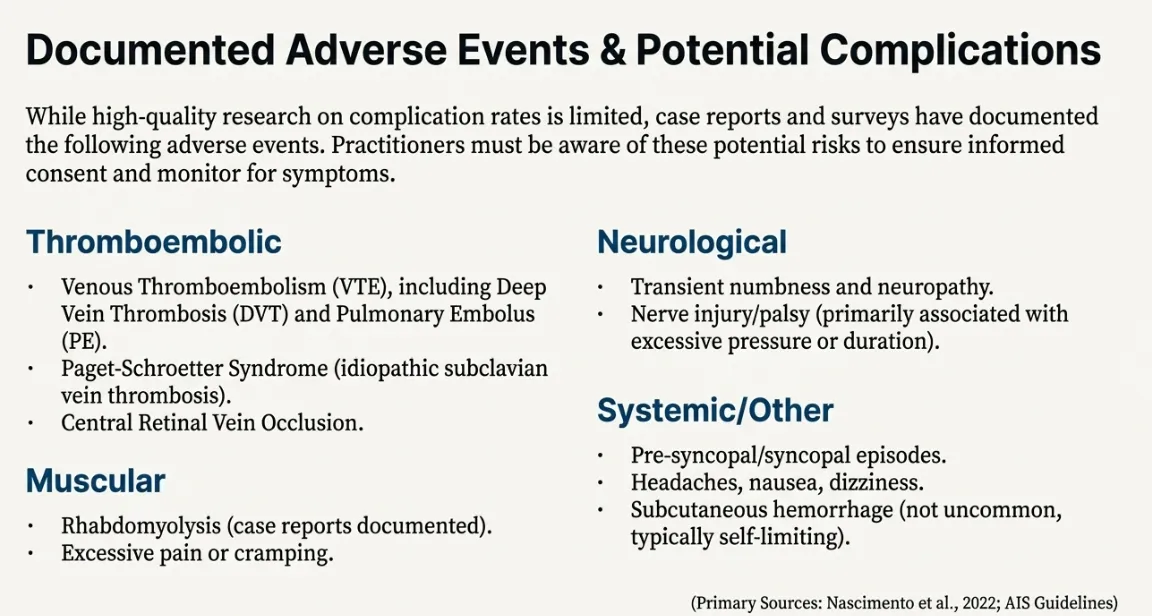
Adverse Event Categories
- Thromboembolic (Very Rare): DVT, PE, superficial thrombophlebitis
- Muscular (Uncommon): Rhabdomyolysis, excessive DOMS, compartment syndrome
- Neurological (Rare): Transient paresthesia, nerve compression symptoms
- Systemic (Minor): Dizziness, nausea, transient hypertension
Note: Most adverse events occur with improper technique, excessive pressures, or inadequate screening.
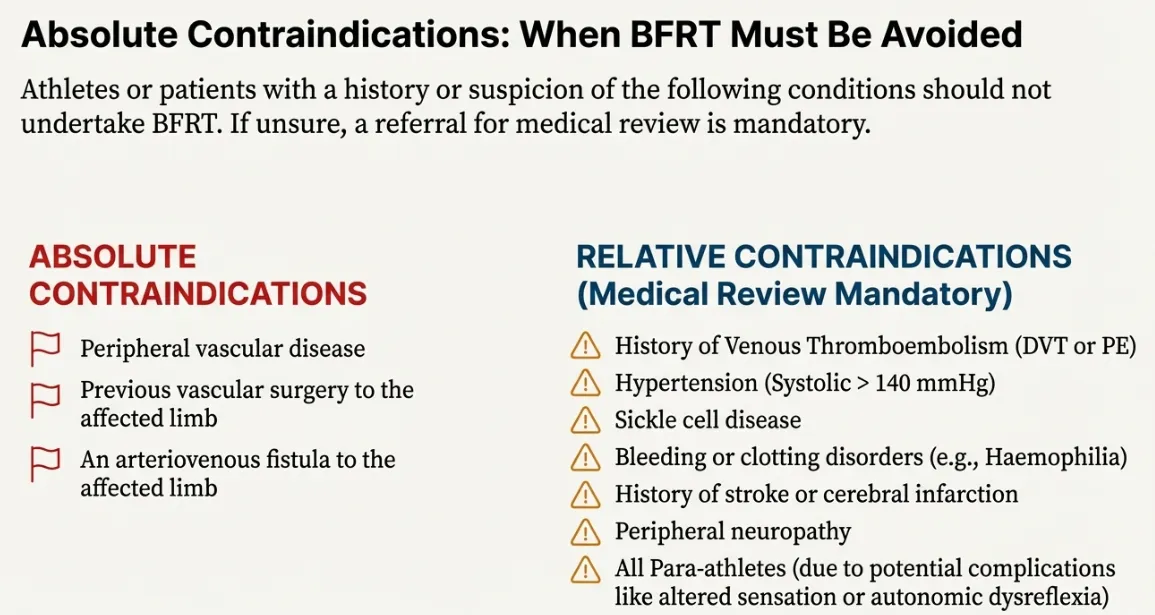
Who Should NOT Use BFRT
Absolute Contraindications (Red Flags):
- Personal history of DVT or PE
- Known clotting disorders (Factor V Leiden, thrombophilia)
- Severe uncontrolled hypertension (>180/110 mmHg)
- Open wounds, infections, or active cellulitis at cuff site
Relative Contraindications (Medical Review Required):
- Cardiovascular disease history
- Pregnancy or early postpartum period
- Significant varicose veins or lymphedema
- Active cancer treatment
- Peripheral neuropathy or vascular disease
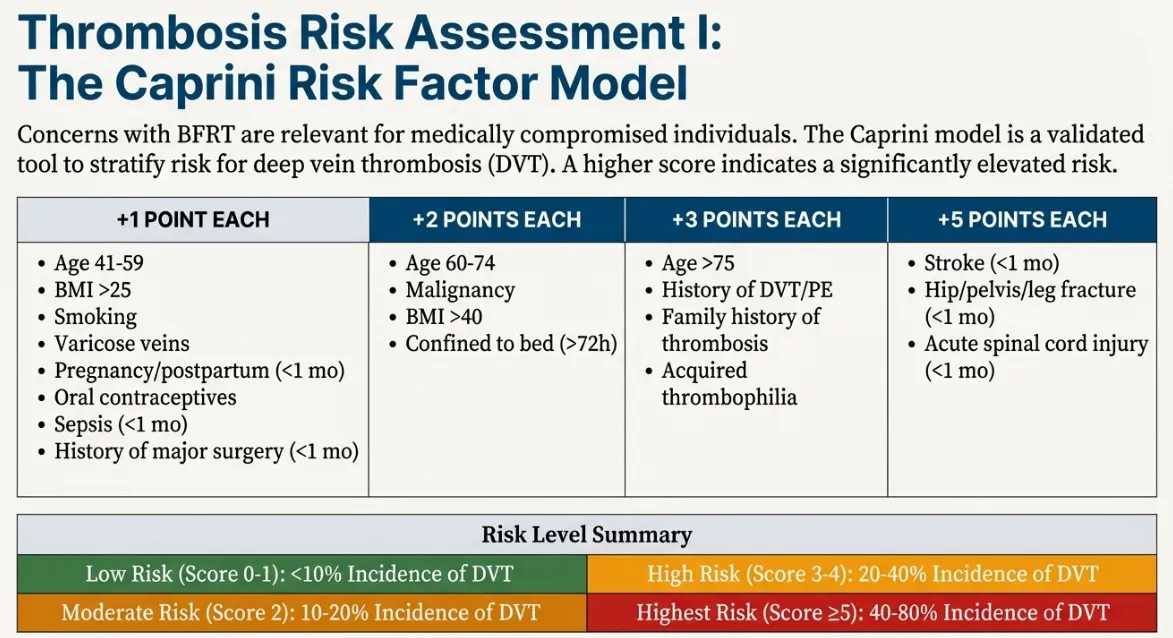
Thrombosis Risk Assessment Tools
Given that thromboembolic events represent the most serious potential complication of BFRT, systematic risk assessment for deep vein thrombosis (DVT) and venous thromboembolism (VTE) is essential for all candidates. Two validated clinical tools are recommended:
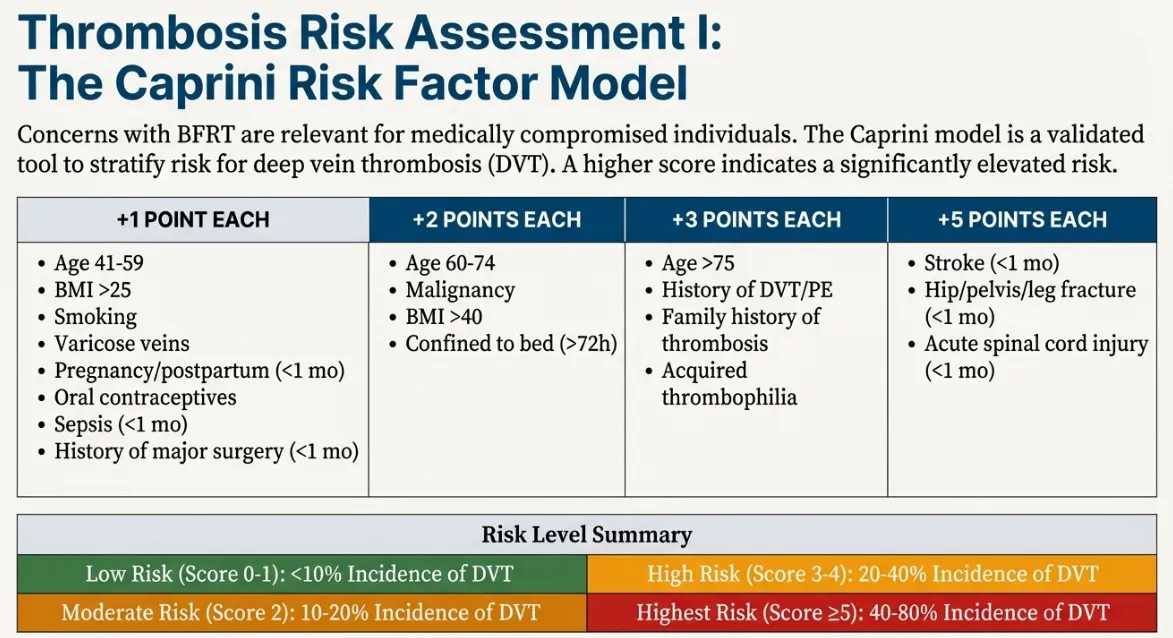
About the Caprini Score
The Caprini Risk Assessment Model is a validated tool for stratifying VTE risk based on cumulative clinical factors. It assigns points for various risk factors, with higher scores indicating elevated thrombosis risk.
How to Use
- Review all risk factors with the patient
- Add points for each applicable factor
- Calculate total score
- Interpret risk category
Risk Categories
- 0-2 points: Low risk - BFRT generally safe with standard precautions
- 3-4 points: Moderate risk - Proceed with enhanced monitoring
- 5-6 points: High risk - Medical clearance required
- 7+ points: Very high risk - BFRT contraindicated or only with physician supervision
For BFRT candidates, we recommend physician consultation for scores ≥5.
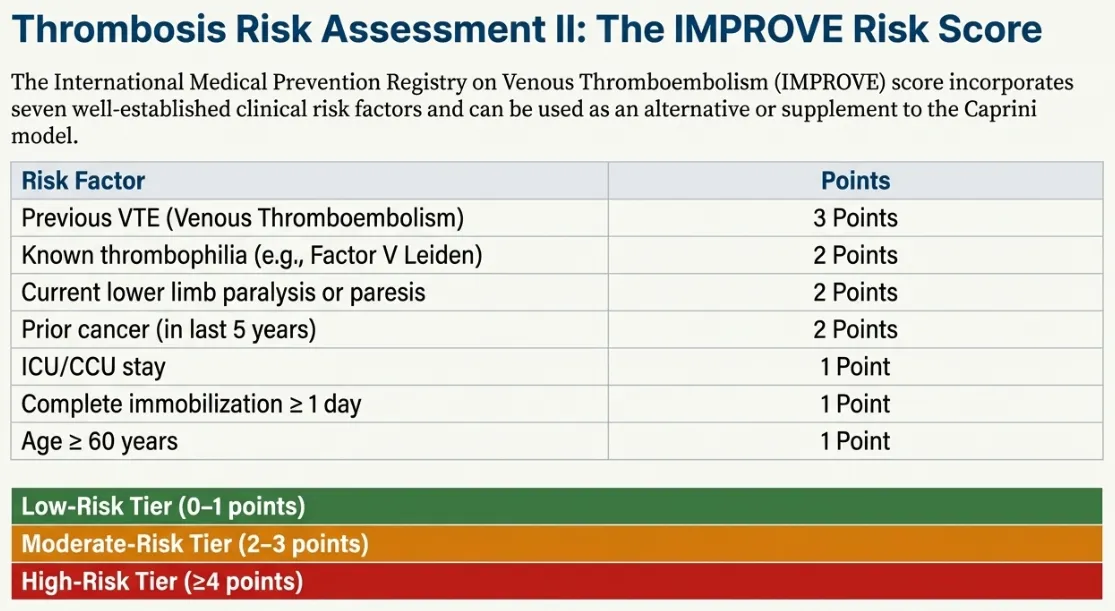
About the IMPROVE Score
The IMPROVE VTE Risk Score was specifically developed to predict venous thromboembolism risk in hospitalized medical patients. While BFRT candidates are typically not hospitalized, this tool is valuable for assessing baseline VTE risk.
Key Risk Factors
- Previous VTE: Highest weighted factor (3 points)
- Known thrombophilia: 2 points
- Current cancer: 2 points
- Immobilization (≥7 days): 1 point
- ICU/CCU admission: 1 point
- Age >60 years: 1 point per decade
Interpretation for BFRT
Score 0-1: Low risk - BFRT safe with standard protocols
Score 2-3: Moderate risk - Enhanced screening and monitoring
Score ≥4: High risk - BFRT requires medical supervision or may be contraindicated
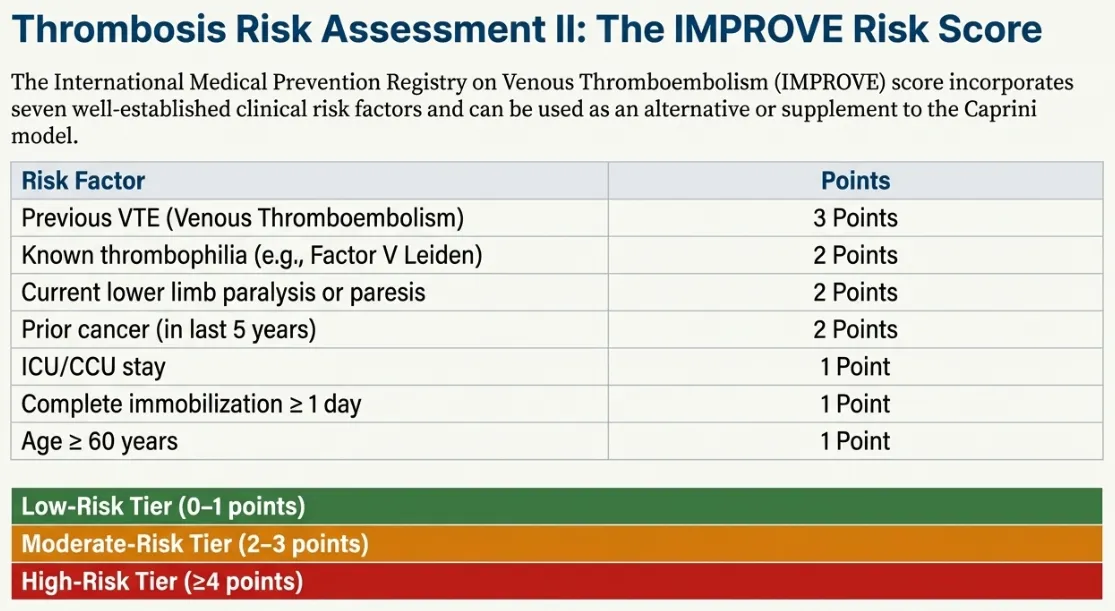
Caprini vs. IMPROVE: Tool Comparison
| Feature | Caprini Score | IMPROVE Score |
|---|---|---|
| Primary Use | Surgical/perioperative VTE risk | Medical patient VTE risk |
| Factors Assessed | 40+ risk factors (comprehensive) | 7 key risk factors (focused) |
| Complexity | More detailed, takes longer | Quick, streamlined assessment |
| Best For BFRT | Post-surgical rehabilitation patients | General fitness/athletic populations |
| Validation | Extensively validated in surgery | Validated in medical inpatients |
Clinical Recommendation: Use Caprini for post-operative patients and those with complex medical histories. Use IMPROVE for quicker screening of generally healthy athletic populations. When in doubt, use both tools.
Comprehensive Screening Protocols
Systematic pre-participation screening is the foundation of safe BFRT implementation. This section provides detailed protocols for risk stratification and special population screening.
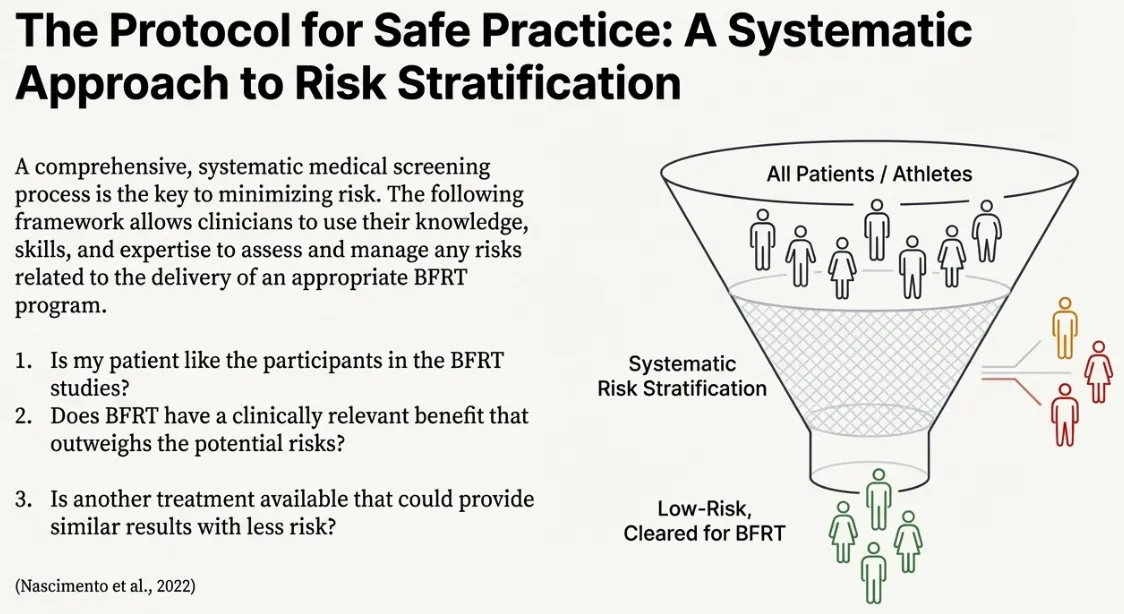
The Five-Stage Screening Funnel
Stage 1: Initial Health History
Comprehensive questionnaire covering:
- Personal and family history of blood clots (DVT/PE)
- Known clotting disorders or thrombophilia
- Cardiovascular disease history
- Current medications (anticoagulants, hormones)
- Recent surgeries or immobilization
- Cancer history or active treatment
Stage 2: Absolute Contraindication Check
STOP immediately if any present:
- Personal DVT/PE history → BFRT contraindicated
- Known clotting disorder → BFRT contraindicated
- Severe hypertension (>180/110) → Control first
- Active infection/wound at cuff site → Wait for healing
Stage 3: VTE Risk Scoring
Apply Caprini or IMPROVE score:
- Low risk: Proceed to Stage 4
- Moderate risk: Enhanced monitoring protocols
- High risk: Physician clearance required
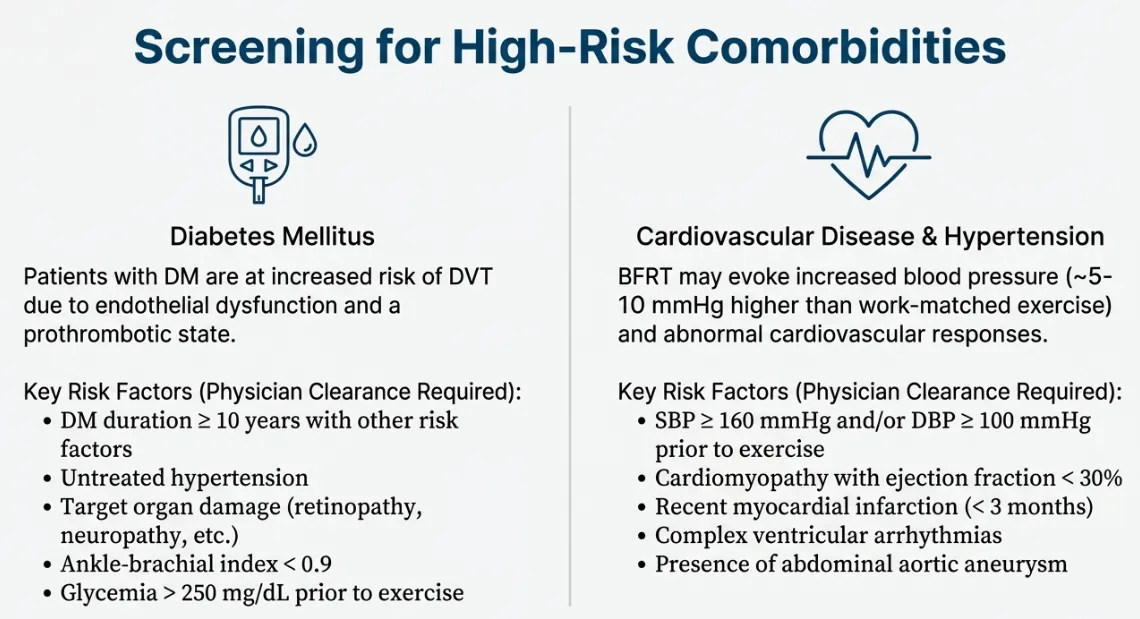
Stage 4: Comorbidity Assessment
Detailed evaluation for:
- Diabetes mellitus (see Figure 10)
- Cardiovascular disease
- Peripheral vascular disease
- Neurological conditions
Stage 5: Clinical Examination
Physical assessment including:
- Resting blood pressure
- Limb circumference measurements
- Skin integrity check
- Peripheral pulse assessment
- Sensation testing (light touch, proprioception)
Final Clearance Decision
✓ Low Risk: Standard BFRT protocols, routine monitoring
⚠ Moderate Risk: Modified protocols, enhanced monitoring, conservative progression
✗ High Risk: BFRT contraindicated OR physician-supervised only
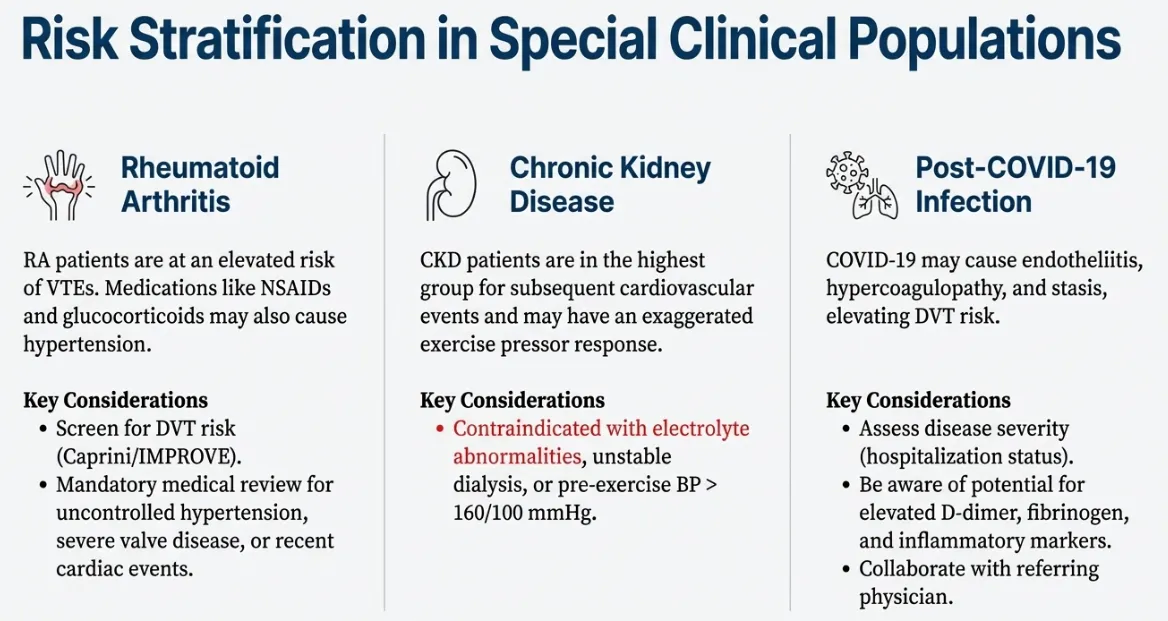
Rheumatoid Arthritis (RA) Patients
Considerations:
- Joint inflammation: Active synovitis may increase discomfort
- Disease activity: BFRT best during remission or low disease activity
- Medication effects: Immunosuppressants may affect healing
- Vasculitis risk: Rare but monitor for vascular complications
Modified Protocol:
- Use lower occlusion pressures (40-50% AOP vs. standard 60-80%)
- Avoid cuff placement over actively inflamed joints
- Shorter occlusion times (10-15 minutes maximum)
- Monitor for increased joint pain or swelling post-session
- Coordinate with rheumatologist for disease flare management
Chronic Kidney Disease (CKD) Patients
Critical Precautions:
⚠️ ABSOLUTE RULE: NEVER apply BFRT cuffs to the arm with an arteriovenous (AV) fistula or dialysis access. Protecting vascular access is paramount.
Additional Considerations:
- Fluid status: Avoid BFRT during volume overload or significant edema
- Electrolyte balance: Ensure normal potassium levels (K+ 3.5-5.0 mEq/L)
- Anemia: Common in CKD—monitor for excessive fatigue
- Timing: Schedule BFRT on non-dialysis days when possible
- Blood pressure: Enhanced monitoring (CKD patients often hypertensive)
Clearance Requirements:
- Nephrologist approval required
- Recent labs (CBC, CMP, eGFR)
- Stable disease (not progressing rapidly)
- Stage 3-4 CKD: Enhanced monitoring
- Stage 5/Dialysis: Only with physician supervision
Post-COVID-19 / Long COVID Patients
Emerging Considerations:
- Cardiovascular effects: Myocarditis, pericarditis risk
- Exercise intolerance: Post-exertional malaise common
- Autonomic dysfunction: POTS-like symptoms, tachycardia
- Hypercoagulable state: Increased VTE risk post-COVID
- Deconditioning: Extended illness leads to muscle loss
Modified Approach:
- Delay BFRT: Wait minimum 3-4 weeks after acute illness resolution
- Cardiac clearance: Especially if hospitalized or severe COVID
- Conservative progression: Start with very low volumes
- Symptom-based progression: Not time-based
- Heart rate monitoring: Stay below 60-70% predicted max initially
- Elevated VTE screening: Use IMPROVE score, consider D-dimer
Clinical Pearl
For special populations, BFRT's ability to achieve muscle growth at low loads is especially valuable—but this benefit must be balanced against heightened physiological vulnerability. When in doubt, start conservatively and progress slowly.
Safe Implementation: The AIS Blueprint
The Australian Institute of Sport (AIS) has published comprehensive guidelines for BFRT implementation that represent the international gold standard for safe, evidence-based application. These protocols form the foundation of our recommendations.
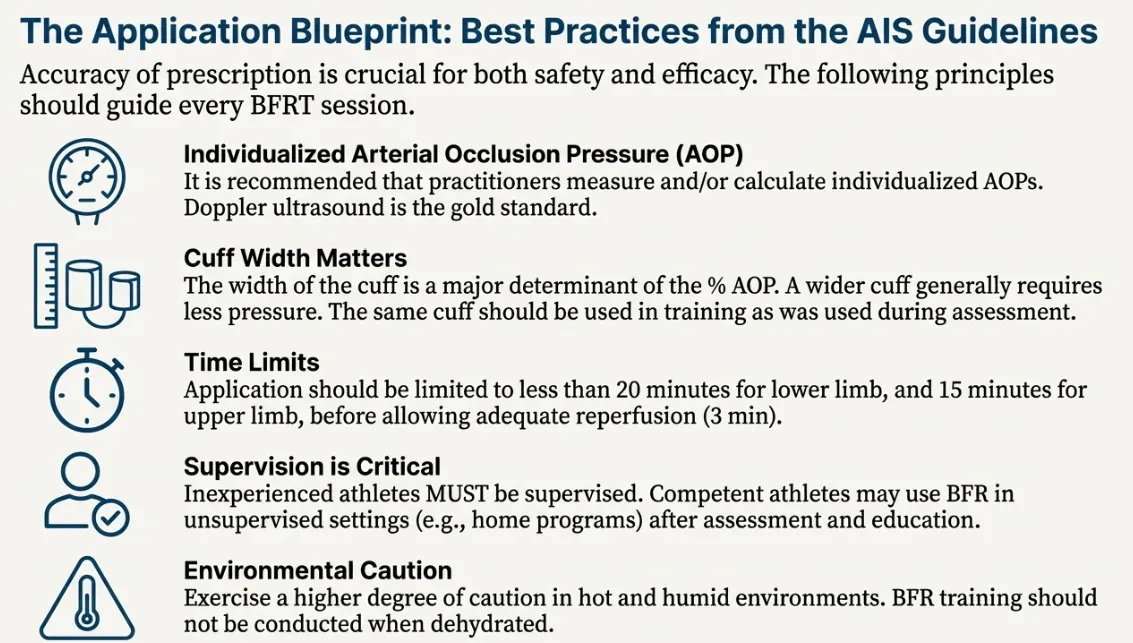
Principle 1: Individualized AOP/LOP Measurement
Non-negotiable requirement: Every individual must have their Arterial (or Limb) Occlusion Pressure measured before training.
Why Individualization Matters
Limb Occlusion Pressure varies significantly between individuals based on:
- Limb circumference: Larger limbs require higher pressures
- Body composition: Adipose tissue affects pressure transmission
- Blood pressure: Systemic BP influences local occlusion
- Cuff width: Wider cuffs occlude at lower pressures
- Age and vascular compliance: Older individuals may have different requirements
Critical Safety Point: Using arbitrary, one-size-fits-all pressures (e.g., "inflate to 200 mmHg") is unsafe and may result in either excessive pressure (risk of adverse events) or insufficient pressure (no training effect).
How to Measure AOP/LOP
Gold Standard Method: Doppler ultrasound
- Apply cuff to proximal limb (upper arm or upper thigh)
- Locate distal pulse with Doppler probe
- Gradually inflate cuff while monitoring pulse signal
- Note pressure at which pulse disappears = AOP/LOP
- Deflate immediately after measurement
Practical Alternative: Digital pressure gauge with pulse sensor (e.g., professional BFR cuffs with automated LOP detection)
Training Pressure Calculation
Once LOP is measured, training pressure is prescribed as a percentage:
- Upper extremity: 40-80% of LOP (typically 50-60% for beginners)
- Lower extremity: 40-80% of LOP (typically 60-70% for beginners)
- Never use 100% LOP: Complete occlusion is unnecessary and increases risk
Principle 2: Appropriate Cuff Width
Scientific evidence clearly demonstrates that cuff width is a critical safety factor:
- Minimum width: 5 cm (wider is safer)
- Recommended: 10-13 cm for clinical/professional use
- Why wider is better: Achieves occlusion at lower absolute pressures, reducing cardiovascular strain
- Avoid elastic bands: No pressure measurement capability, unpredictable occlusion
Our wide-fabric BFR training cuffs meet clinical standards with 10-13cm width for both upper and lower extremities, ensuring safe occlusion at lower pressures.
Principle 3: Time Limits
Maximum continuous occlusion time:
- Per exercise bout: 5-10 minutes maximum under occlusion
- Rest between sets: Cuffs can remain inflated OR deflated (research supports both)
- Total session time: Generally 15-20 minutes total occlusion time
- Frequency: 2-3 times per week (same as traditional training)
Principle 4: Qualified Supervision
BFRT should be supervised by qualified practitioners:
- Physical therapists
- Athletic trainers
- Exercise physiologists
- Sports medicine physicians
- Certified strength coaches with BFRT training
Principle 5: Environmental Considerations
- Heat: Avoid BFRT in excessive heat—increases cardiovascular strain
- Altitude: Use lower pressures at high altitude (reduced oxygen availability)
- Hydration: Ensure adequate hydration before sessions
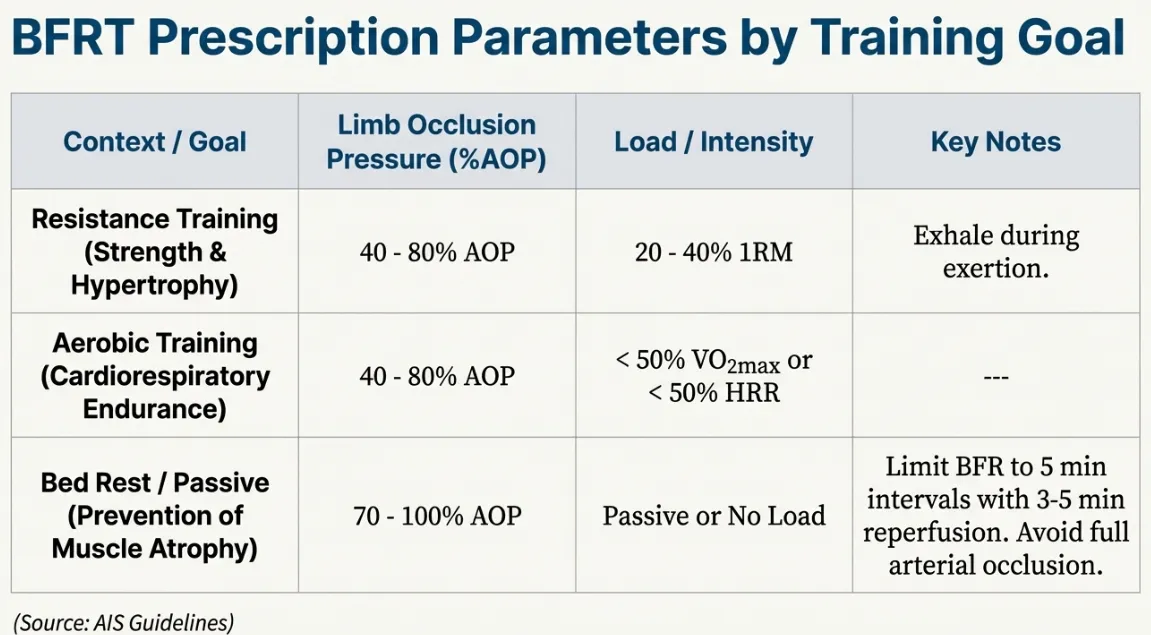
Prescription Parameters by Goal
Muscle Hypertrophy (Most Common Goal)
- Occlusion: 40-80% LOP (50-60% for beginners)
- Load: 20-40% 1RM
- Volume: 4 sets × 15-30 reps (75 total reps target)
- Rest: 30 seconds between sets (short rest amplifies metabolic stress)
- Tempo: Controlled 2-0-2 (2 sec concentric, 0 pause, 2 sec eccentric)
- Frequency: 2-3x/week per muscle group
Strength Development
- Occlusion: 60-80% LOP (higher pressure)
- Load: 30-50% 1RM (slightly heavier than hypertrophy)
- Volume: 3-4 sets × 8-15 reps
- Rest: 60 seconds (longer rest for strength focus)
- Note: Some protocols combine BFRT with heavy load training
Rehabilitation/Post-Surgical
- Occlusion: 40-60% LOP (conservative)
- Load: 10-30% 1RM (very light loads tolerable post-surgery)
- Volume: 3-4 sets × 15-30 reps
- Rest: 30-60 seconds
- Progression: Symptom-based, not time-based
- Medical clearance: Required post-operatively
Aerobic/Walking Enhancement
- Occlusion: 40-50% LOP (lower than resistance training)
- Intensity: Low-moderate walking pace
- Duration: 5-20 minutes continuous or intermittent
- Application: Particularly valuable for elderly populations
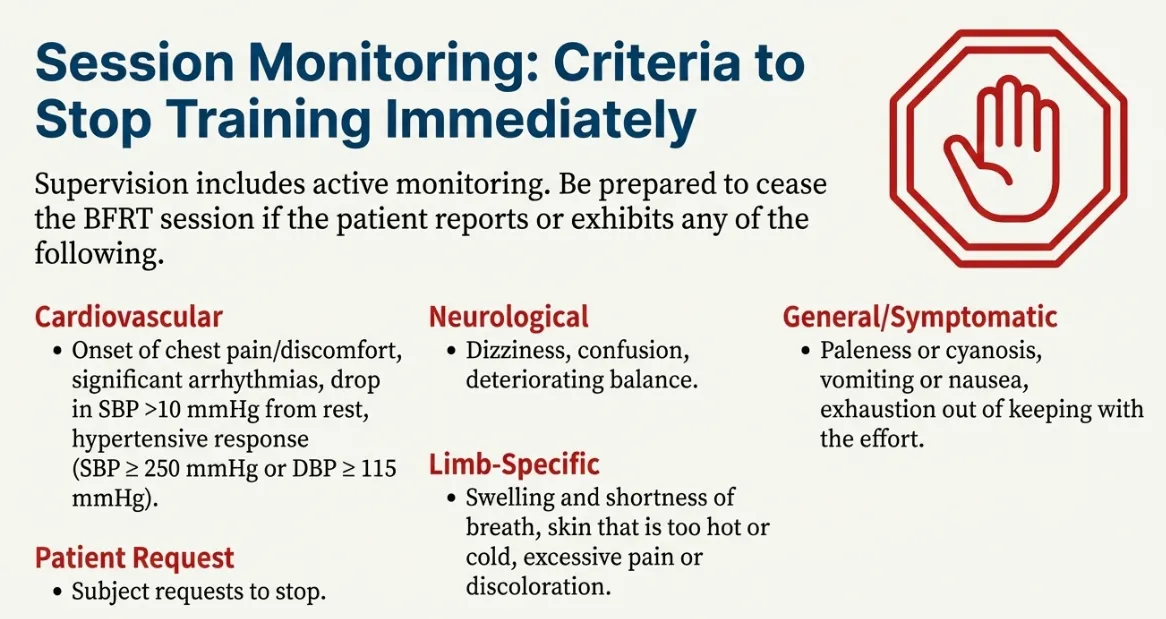
Session Monitoring & Stop Criteria
Real-time monitoring during BFRT sessions is essential for detecting early warning signs and preventing adverse events. This section provides comprehensive monitoring protocols and absolute stop criteria.
Pre-Session Assessment
Before every BFRT session:
- Resting BP: Should be <180/110 (severe hypertension contraindicated)
- Resting HR: Baseline measurement for during-session comparison
- Symptom check: Any new symptoms since last session?
- Medication changes: New anticoagulants, BP meds?
- Recent illness/injury: DVT/surgery/trauma?
- Sleep/hydration: Adequate rest and fluid intake?
During-Session Monitoring
Cardiovascular Monitoring
Monitor continuously for:
- Heart rate: Should stay <85% age-predicted max with low-load BFRT
- Blood pressure: Check mid-session and with any symptoms
- Chest discomfort: Any pressure, tightness, or pain
- Dyspnea: Difficulty breathing beyond normal exertion
🛑 STOP immediately if:
- Chest pain or pressure
- Severe dyspnea
- BP >200/110 mmHg
- HR >85% max (sustained)
Neurological Monitoring
Assess for:
- Pain quality: Normal training discomfort vs. sharp, severe pain
- Paresthesia: Numbness, tingling, "pins and needles"
- Motor function: Weakness beyond normal fatigue
- Proprioception: Loss of position sense
🛑 STOP immediately if:
- Severe, sharp, or stabbing pain
- Numbness or complete loss of sensation
- Weakness that prevents movement
- Persistent paresthesia during rest periods
Limb-Specific Indicators
Visual inspection for:
- Swelling: Moderate "pump" is normal; excessive edema is not
- Color changes: Slight redness OK; pallor or cyanosis (blue) not OK
- Capillary refill: Press nail bed, should reperfuse in <2-3 seconds
- Skin temperature: Cool skin may indicate excessive occlusion
🛑 STOP immediately if:
- Severe swelling (>2× normal pump)
- Cyanosis (bluish discoloration)
- Pallor (excessive paleness)
- Capillary refill >3 seconds
General/Systemic Symptoms
Monitor for:
- Nausea: Mild nausea may occur; severe is concerning
- Dizziness: Lightheadedness, presyncope
- Visual changes: Blurred vision, tunnel vision
- Excessive fatigue: Beyond normal training fatigue
🛑 STOP immediately if:
- Severe nausea or vomiting
- Presyncope or syncope
- Visual disturbances
- Patient requests to stop
Post-Session Assessment
- Immediate cuff removal: Deflate and remove after final set
- BP recovery: Should return to near-baseline within 5-10 minutes
- Limb assessment: Pulse present, normal color, sensation intact
- Symptom resolution: Numbness, discomfort should resolve quickly
- 24-hour follow-up: Contact patient to assess for delayed symptoms
⚠️ Emergency Response Protocol
If serious adverse event occurs:
- Immediately deflate and remove cuffs
- Place patient in safe position (supine if dizzy, semi-recumbent if dyspneic)
- Assess vital signs (BP, HR, respiratory rate)
- Call emergency services if: chest pain, severe dyspnea, loss of consciousness, suspected DVT
- Monitor continuously until symptoms resolve or EMS arrives
- Document incident thoroughly
- Notify supervising physician
Conclusion: Harnessing BFRT Power Responsibly
Blood Flow Restriction Training stands at the intersection of remarkable efficacy and serious responsibility. The same physiological mechanisms that enable muscle growth at 20-30% 1RM—metabolic stress, accelerated fiber recruitment, anabolic signaling—also create a unique stress environment that requires disciplined, evidence-based application.
Key Takeaways
1. Safety Through Science
BFRT is not dangerous when applied correctly. Systematic reviews show adverse event rates comparable to traditional exercise in properly screened populations. The key is adherence to protocols:
- Comprehensive pre-participation screening
- Risk stratification using validated tools
- Absolute respect for contraindications
- Medical clearance for high-risk populations
2. Individualization is Non-Negotiable
There is no "one size fits all" in BFRT:
- Every person has unique Limb Occlusion Pressure
- Training pressure must be individualized (% of LOP)
- Comorbid populations require modified protocols
- Progression must be symptom-based, not standardized
3. Monitoring Prevents Complications
Most adverse events are preventable through vigilant monitoring:
- Pre-session screening catches contraindications
- During-session assessment detects early warning signs
- Immediate response to stop criteria prevents serious events
- Post-session follow-up identifies delayed complications
4. Education Enables Excellence
Practitioners must commit to ongoing education:
- Formal BFRT certification courses
- Understanding underlying physiology
- Staying current with evolving research
- Networking with experienced BFRT clinicians
Moving Forward with Confidence
This guide has equipped you with comprehensive knowledge to implement BFRT safely and effectively. The protocols presented represent current best practices synthesized from international guidelines (AIS), systematic reviews, and clinical experience. Learn more about the science behind blood flow restriction training and how it achieves remarkable results with minimal load.
When screening is thorough, protocols are individualized, and monitoring is diligent, BFRT becomes a powerful tool that expands what's possible in rehabilitation, performance enhancement, and healthy aging.
Resources for Continued Learning
- Certification Courses: Comprehensive BFRT training programs
- Professional Equipment: BFR Cuffs Complete Kit for occlusion training with digital pressure gauge and wide pneumatic cuffs
- Clinical Support: Consultation services for complex cases
- Research Updates: Subscribe to our newsletter for latest findings
- Learn More: Explore the benefits of BFR training for rehabilitation and performance
Ready to Implement BFRT?
Equip your practice with professional-grade equipment and certification:
Frequently Asked Questions
No, BFRT is not inherently dangerous when applied correctly. Systematic reviews analyzing thousands of BFRT sessions show that adverse event rates are comparable to traditional resistance training in properly screened populations. The key factors that ensure safety are:
- Comprehensive pre-participation screening to identify contraindications
- Individualized pressure prescription based on measured LOP (not arbitrary pressures)
- Use of appropriate equipment (wide pneumatic cuffs with pressure gauges)
- Qualified practitioner supervision
- Real-time monitoring and adherence to stop criteria
Most reported adverse events occurred with improper application—excessive pressures, inadequate screening, or use of inappropriate equipment (e.g., elastic bands without pressure measurement).
Documented risks, while rare, include:
- Thromboembolic events: DVT/PE (very rare, primarily in individuals with pre-existing risk factors)
- Muscular complications: Excessive delayed-onset muscle soreness (DOMS), very rarely rhabdomyolysis
- Neurological symptoms: Transient numbness/tingling (usually resolves immediately upon cuff removal)
- Cardiovascular stress: Temporary blood pressure elevation (greater in those with hypertension)
The incidence of serious adverse events is estimated at <1% when proper protocols are followed, and most minor symptoms (mild tingling, transient dizziness) resolve immediately upon cuff deflation.
Absolute Contraindications (NEVER use BFRT):
- Personal history of deep vein thrombosis (DVT) or pulmonary embolism (PE)
- Known clotting disorders (Factor V Leiden, thrombophilia, antiphospholipid syndrome)
- Severe uncontrolled hypertension (≥180/110 mmHg)
- Open wounds, active infections, or cellulitis at cuff application site
- Recent acute cardiovascular event (MI, stroke within 6 months)
Relative Contraindications (Require medical clearance):
- Cardiovascular disease (especially if symptomatic)
- Pregnancy or early postpartum period
- Varicose veins, lymphedema, or peripheral vascular disease
- Active cancer or recent cancer treatment
- Peripheral neuropathy
- Chronic kidney disease (especially with AV fistula)
Safe, effective BFR pressure MUST be individualized based on your measured Limb Occlusion Pressure (LOP) or Arterial Occlusion Pressure (AOP). Professional BFR equipment with digital pressure gauges makes this measurement accurate and repeatable. Here's how:
- Measure your LOP: Using a Doppler ultrasound or automated tourniquet system, determine the pressure at which arterial blood flow to the limb is completely occluded
- Calculate training pressure: Use a percentage of your LOP:
- Upper extremity: 40-80% LOP (50-60% for beginners)
- Lower extremity: 40-80% LOP (60-70% for beginners)
- Example: If your measured arm LOP is 150 mmHg, your training pressure would be 75-90 mmHg (50-60% of 150)
NEVER use arbitrary pressures (e.g., "inflate to 200 mmHg") without measuring LOP. Limb occlusion pressure varies dramatically between individuals based on limb size, body composition, blood pressure, and cuff width. What's safe for one person may be dangerously high or ineffectively low for another.
Recommended time limits:
- Initial screening and clearance by qualified healthcare professional
- Professional BFR education or training (ideally certification course)
- Proper equipment: Wide pneumatic occlusion cuffs with digital pressure gauge
- Individualized LOP measurement completed by professional
- Low-risk health profile (no contraindications or significant comorbidities)
- Knowledge of monitoring parameters and stop criteria
- Individuals with cardiovascular disease, diabetes, or other comorbidities (require ongoing professional supervision)
- Post-surgical rehabilitation (should be supervised by PT)
- Those unable to measure their own LOP or purchase appropriate equipment
- Anyone using improvised equipment (elastic bands, knee wraps, etc.)
Can I do BFR training at home without supervision?
Home use is possible BUT requires meeting specific conditions:
Prerequisites for unsupervised home BFRT:
NOT appropriate for home use:
Our recommendation: Begin BFRT under qualified supervision, complete formal education, and transition to supervised home use only after demonstrating competency and safety awareness.
Implement BFRT Safely in Your Practice
Equip yourself with professional-grade equipment and comprehensive education to deliver the benefits of BFRT with confidence.
Professional-grade equipment backed by science. Safe, effective, and built to last.
Medical Disclaimer
This guide is for educational purposes and is not a substitute for professional medical advice, diagnosis, or treatment. Blood Flow Restriction Training should only be performed after appropriate screening and under qualified supervision. Always consult with a healthcare provider before beginning any new exercise program, especially if you have pre-existing medical conditions. The information presented represents current best practices but may not apply to all individuals or circumstances. Individual results and safety profiles may vary.